Rheumatism treatment Vienna
Rheumatism is generally a long-term, progressive and disabling disease associated with pain of the musculoskeletal system. This disease gradually limits a person’s mobility and prevents them from performing normal daily activities and living an independent and self-sufficient life. Although rheumatism is the common disease of the joints, the disease can also affect any other organ in the body, such as the lungs, heart or eyes. Of the joints, the joints on hands are most often affected.
Rheumatic diseases and their triggers
The original causes that lead to the development of the disease in a particular person are not yet known. However, we have many clues about the mechanisms by which the disease damages the joints and causes the typical complaints of rheumatism patients. The most important harmful process is chronic joint inflammation. This is caused by white blood cells invading the joint and manifests as swelling, heat, tenderness to touch, pain and limited functionality. After some time, the persistent inflammation leads to the destruction and deformation of the joint. Here, the application of therapies is essential.

Restriction of mobility
In more than half of patients with rheumatic disease, there is involvement of the elbow joint. The importance of this disease in the elbow area is multiplied by the fact that its mobility is limited at a very early stage, either because of pain or because of the considerable aggressiveness of the rheumatic process. As a result, in the early stages of the disease, the patient often suffers from limited upper extremity functionality caused not only by the elbow joint itself, but also by the inability to position the hand effectively in space. Therefore, even with preservation of hand function, a patient with elbow joint motion restriction is unable to perform normal activities of daily living, especially eating and personal hygiene.
Different types of rheumatism
Different types of rheumatism
Basically, two types of elbow joint involvement due to the rheumatic process are encountered in clinical practice. More common is restriction of joint motion of varying degrees to complete immobility of the joint. The position in which stiffness occurs in rheumatism is usually functionally disadvantageous. The second, less common type of disability is an unstable, wobbly elbow joint. The degree of instability can vary from mild wobbliness to dislocation.

Rheumatoid arthritis
Rheumatoid arthritis is a chronic inflammatory autoimmune disease that primarily affects the joints. It is characterized by pain, swelling and stiffness of the affected joints. However, rheumatoid arthritis can also affect other organs and systems in the body, such as the skin, eyes and cardiovascular system. Rheumatoid arthritis occurs when the immune system mistakenly attacks healthy joints and triggers an inflammatory response. The exact cause is not yet fully understood, but both genetic and environmental factors are thought to play a role. Rheumatoid arthritis treatment aims to reduce inflammation, relieve pain and preserve joint function. This can be achieved through medication, physical therapy and lifestyle changes. Early diagnosis and treatment by rheumatologists and physicians is critical to slowing the progression of the disease and minimizing damage to the joints.
Symptoms of rheumatic disease
Pressure pain, swelling of the joint and increased skin temperature dominate. Irritation of the elbow nerve may occur. Involvement of the joint between the radius and ulna results in pain and possible stiffness on forearm rotations.
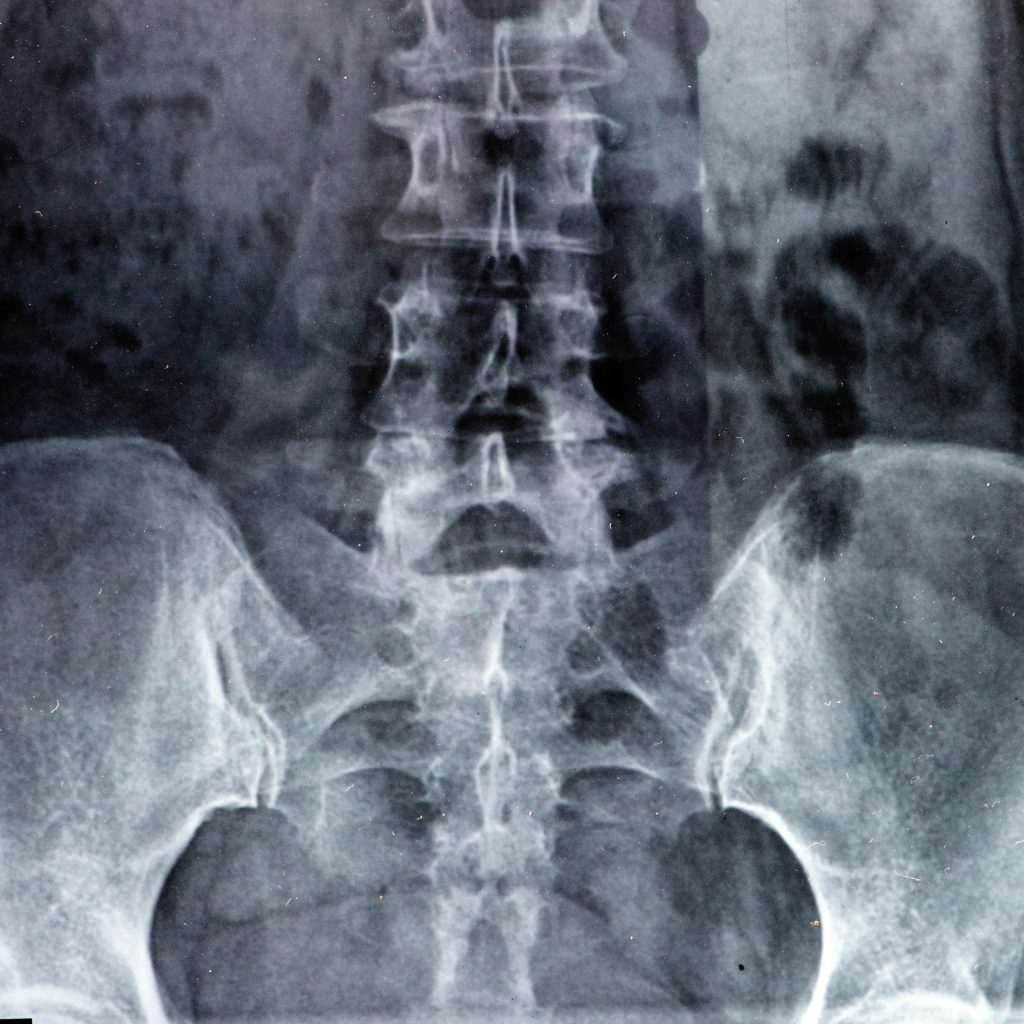
Diagnosis of rheumatic diseases
The diagnosis of rheumatic diseases, including rheumatoid arthritis, usually requires a comprehensive evaluation by a rheumatologist, a specialist in rheumatology. The diagnostic process usually begins with a detailed history, during which the affected person is informed about his or her symptoms, duration and course. The doctor will also ask about possible risk factors and family history. A physical examination is then performed, during which the physician looks for signs of inflammation, swelling, redness, and limited joint mobility. Various diagnostic tests can be used to confirm the diagnosis and rule out other possible causes. These include blood tests to examine inflammatory markers such as C-reactive protein (CRP) and rheumatoid factors. Imaging techniques such as X-rays, ultrasound and magnetic resonance imaging (MRI) may also be used to more accurately assess joints and their damage. In some cases, a joint puncture may also be performed, in which fluid is removed from an inflamed joint and examined in the laboratory. The diagnosis of rheumatic diseases often requires a comprehensive interaction of all these diagnostic approaches to obtain an accurate picture of the disease and to develop an appropriate treatment strategy.
Rheumatism treatment and therapy by internal medicine
The most important thing in therapy is to prevent major destruction of the cartilage, bone or tissue around the joint in the elbow. It is clear that no method of conservative treatment is sufficiently likely to halt the rheumatic process in the joint. Therefore, close cooperation between rheumatology and orthopedics is extremely important. The basis of local nonoperative treatment is the use of cortisone infiltrations. Cortisone does relieve inflammation in the joint, but only for a short time. However, it is harmful to cartilage and thus to the overall condition of the joint. Therefore, a larger number of cortisone infiltrations is not appropriate.
What to do if the condition worsens?
If the condition of the elbow joint deteriorates despite comprehensive conservative treatment, a surgical solution must be initiated. Basically, possible operations on the elbow joint affected by the rheumatic process can be divided into several types:
- Removal of the head of the radius,
- early removal of inflammatory joint tissue (so-called synovectomy),
- Arthroplasty, today most frequently a total endoprosthesis
- surgical stiffening of the joint (so-called arthrodesis),
- Release of nerves,
- Removal of rheumatic nodules.

Removal of the head of the radius
Many patients with rheumatic diseases in the elbow experience movement restrictions due to destruction of the head of the radius. Contraction of the biceps pulls the radius into the anterior partial dislocation. This restricts the flexion of the elbow. Partial dislocation is made possible by the destruction of ligaments by aggressive rheumatic tissue. In most cases, we combine removal of the proximal end of the radius with removal of the aggressive rheumatic tissue (synovectomy), which delays destruction of the entire joint.

Endoprothresis for rheumatic diseases of the elbow
In certain cases, the removed head of the radius can be replaced with an endoprosthesis. Replacement of the storage head (on the outer side) helps to restore the physiological distribution of forces in the elbow joint, thus reducing the risk of overloading the inner side of the joint affected by the rheumatic process. The surgical procedure for salivary head removal sometimes includes careful reconstruction of the ligamentous apparatus. This prevents the complication of occurrence of partial dislocation of the joint.
Removal of inflammatory joint tissue (synovectomy)
Early synovectomy is indicated if swelling, pain, or morning stiffness do not resolve after four to six months despite intensive conservative treatment. Delaying synovectomy is not appropriate for the elbow joint because of its tendency to restrict motion early. At the elbow, late synovectomy has no major significance and we perform it only in exceptional cases. Thus, it is a preventive procedure that, when properly timed, can significantly reduce the risk of joint destruction from the rheumatic process. We usually combine synovectomy of the elbow joint with removal of the salivary head.

Arthroplasty (total endoprosthesis)
The removal of joint surfaces destroyed by rheumatic diseases (so-called arthroplasty) already took place at the turn of the 18. to the 19th century. The result at that time was a relatively painless, mobile, but rather unstable elbow. At 20th century, other tissues (e.g., skin or ligaments) were introduced into the joint and the lateral ligaments were preserved to keep the elbow stable. Nowadays, we perform these operations only when the implantation of an artificial joint is not possible. Implantation of an artificial joint by an internist gradually became the most commonly performed elbow joint arthroplasty. Today, we have modern implants that relieve the patient of pain and restore mobility in the joint and thus self-care.
Stiffening of the joint (arthrodesis)
The indications for arthrodesis of the elbow joint have become very narrow with the development of artificial joints. Arthrodesis can be performed only in severely damaged and wobbly joints in people for whom implantation of an artificial joint is not possible (most often in infectious complications).
Nerve release
Sometimes patients with rheumatism experience compression of an elbow nerve, or more rarely, a spinal nerve (known as Pannas palsy). If the patient’s discomfort is significant, specialists loosen the corresponding nerve.
Removal of rheumatic nodes by rheumatology
Removal of larger rheumatoid nodules located in the posterior aspect of the elbow is considered a clear indication for surgery. The lumps can make it difficult for the patient to rest on the elbow each time and are often painful. Outside the posterior region, another troublesome site is the edge of the proximal ulna and the inner side of the humerus, from where we remove rheumatoid nodules. Our team usually operates on an outpatient basis as part of day surgery under local anesthesia.
